Researchers with Sylvester Comprehensive Cancer Center and the University of Miami have developed an innovative strategy to help predict COVID-19 outbreaks up to four days before individual tests positive for the disease. And this early warning system could prove even more useful as the Delta variant is prompting a surge in coronavirus cases.
Researchers with Sylvester Comprehensive Cancer Center and the University of Miami have developed an innovative strategy to help predict COVID-19 outbreaks up to four days before individual tests positive for the disease. And this early warning system could prove even more useful as the Delta variant is prompting a surge in coronavirus cases.
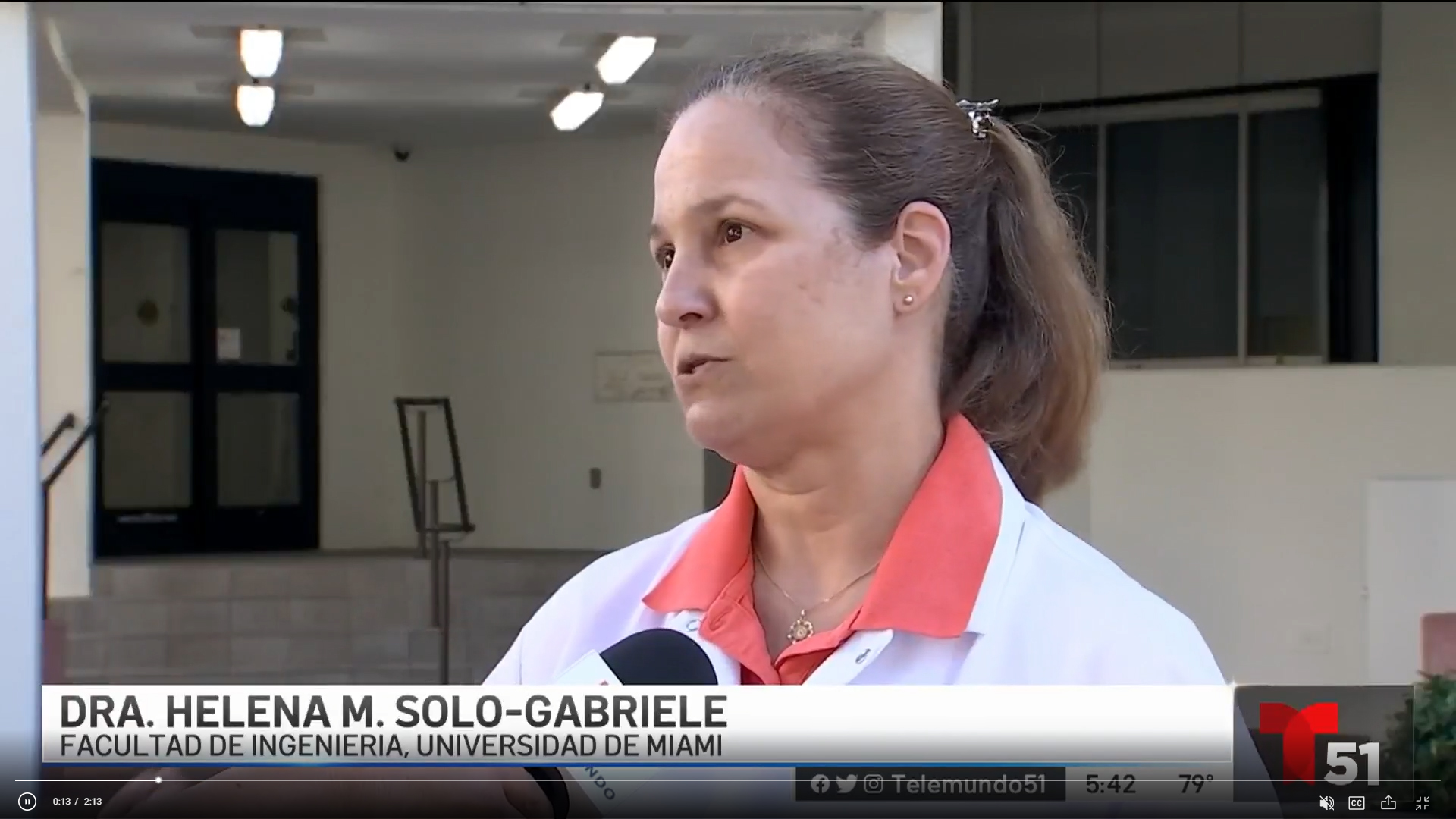
 “This knowledge could be invaluable to protecting our students, staff, faculty, and hopefully, our communities,” says Helena Solo-Gabriele, an environmental engineering professor who began the research study last summer with the help of George Grills, Sylvester’s Associate Director of Shared Resources.
“This knowledge could be invaluable to protecting our students, staff, faculty, and hopefully, our communities,” says Helena Solo-Gabriele, an environmental engineering professor who began the research study last summer with the help of George Grills, Sylvester’s Associate Director of Shared Resources.
“By sampling wastewater flowing from campus buildings, Solo-Gabriele says her research team members are now able to isolate areas where SARS-CoV-2—the virus that causes COVID-19—is present on campus. University leaders are now using the data to plan for more COVID-19 testing, to prepare for patients utilizing the Student Health Service, as well as to assess the need for more isolation and quarantine spaces,” says Erin Kobetz, Ph.D., M.P.H., associate director of Population Sciences and Cancer Disparity at Sylvester and Vice Provost for Research and Scholarship at the University of Miami. Dr. Kobetz is leading the University’s COVID-19 testing, tracking, and tracing efforts.
 “This is another data point that’s important for how we assess the level of community transmission of COVID-19 across our university,” Dr. Kobetz adds. “We use it to inform our approach about where there may be a spike and to plan logistically and operationally to support that.”
“This is another data point that’s important for how we assess the level of community transmission of COVID-19 across our university,” Dr. Kobetz adds. “We use it to inform our approach about where there may be a spike and to plan logistically and operationally to support that.”
The COVID-19 wastewater surveillance project, now funded by a $5 million grant from the National Institutes of Health (NIH), grew out of research indicating that humans shed particles of COVID-19 in their urine, feces, and exhaled breath before they even notice symptoms. Initially, Solo-Gabriele’s team investigated whether an early warning model could be created using wastewater. When they learned that asymptomatic carriers of COVID-19 can still infect and sicken others, it catalyzed the project because this indicated that early detection of the virus could help save lives.
Yet through the project, Solo-Gabriele has recognized that wastewater surveillance is useful beyond COVID-19.
“This can help determine the rate at which a community is experiencing disease, and it gives a sense of how many people that contribute to that sewage could be sick,” says Solo-Gabriele, who studies water and beach contamination in South Florida. “Not only for COVID-19, but many other diseases can be monitored this way.”
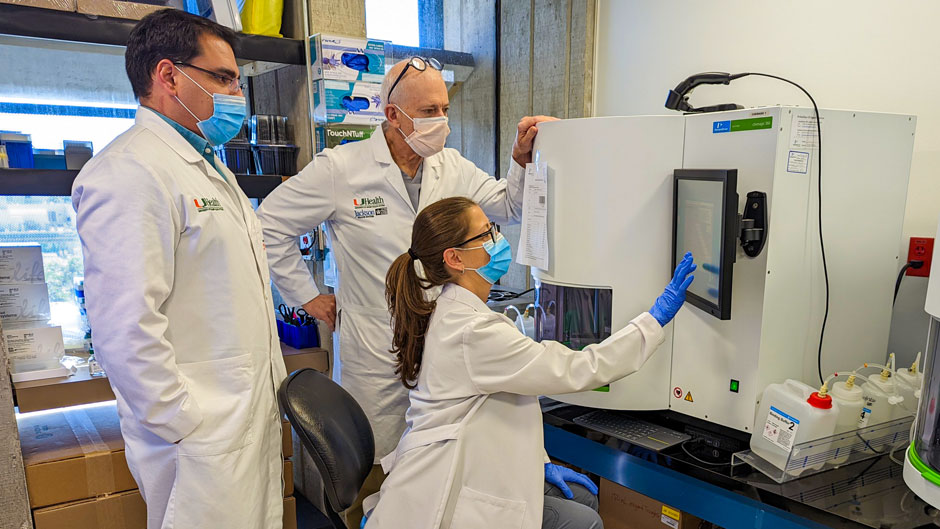
Yet Solo-Gabriele could not do it alone. She quickly met Grills, who connected her with colleagues at the Miller School of Medicine who were already creating tests to identify COVID-19 in patients, to see if the same tests could be adapted to wastewater. As a molecular biologist focused on genetics and genomics, Grills had worked with colleagues at Weill Cornell Medicine to track novel pathogens using surface sampling in urban environments.
Based on research being done around the world, Solo-Gabriele and Grills realized that if researchers at the University could track high virus levels in the wastewater to specific locations, it could help predict the locations of emerging outbreaks.
Their project soon grew into a university-wide effort.
 “We have faculty from all three UM campuses involved in this project, and we are integrating environmental surveillance of the virus with human COVID-19 data to develop a model to predict outbreaks and to inform public health decision making,” Grills says. “The tools and methodologies that we are developing also have the potential to monitor other types of infectious diseases going forward.”
“We have faculty from all three UM campuses involved in this project, and we are integrating environmental surveillance of the virus with human COVID-19 data to develop a model to predict outbreaks and to inform public health decision making,” Grills says. “The tools and methodologies that we are developing also have the potential to monitor other types of infectious diseases going forward.”
While they started with weekly samples, Solo-Gabriele says the NIH funding has allowed the team to expand and collect samples more frequently to see if they can get an even more detailed early warning—perhaps even allowing them to estimate the number of infected people in a building.
She pointed out that the entire process was accelerated by a new analytical technique — developed by Mark Sharkey, assistant professor of research in the Division of Infectious Disease—called V2G (for “volcano second generation”) quantitative polymerase chain reaction (or qPCR) that can pick up COVID-19 in sewage faster than earlier methods.
 In addition, one of the project’s co-investigators, Chris Mason, a professor of physiology and biophysics at Weill Cornell Medicine, and his team also check the wastewater samples for SARS-CoV-2 using a rapid diagnostic tool he developed called loop-mediated isothermal amplification (LAMP). The entire project is outlined in a new paper published recently in the journal Science of the Total Environment.
In addition, one of the project’s co-investigators, Chris Mason, a professor of physiology and biophysics at Weill Cornell Medicine, and his team also check the wastewater samples for SARS-CoV-2 using a rapid diagnostic tool he developed called loop-mediated isothermal amplification (LAMP). The entire project is outlined in a new paper published recently in the journal Science of the Total Environment.
Since it began last summer, the wastewater project has expanded dramatically.
It now collects samples with the help of automated devices from 16 sites across the University’s three campuses. Their typical workflow begins with the sampling team, which includes Solo-Gabriele, students, and research staff, along with the University’s Facilities and Environmental Health and Safety team collecting and filtering the samples, before passing them along to Sharkey, Mason, and Sion Williams at the Onco-Genomics Shared Resource at Sylvester Comprehensive Cancer Center for further analysis.
 Then the wastewater data is analyzed by public health professor Naresh Kumar and research analyst Alejandro Mantero, who correlate it with campus-wide COVID-19 test positivity rates to feed the project’s prediction model. This allows the team to estimate where outbreaks may occur. Kumar says their model now suggests that the virus can be detected up to four days before a clinical diagnosis of COVID-19. It also shows that the virus persists in wastewater up to five days after a positive diagnosis, he added.
Then the wastewater data is analyzed by public health professor Naresh Kumar and research analyst Alejandro Mantero, who correlate it with campus-wide COVID-19 test positivity rates to feed the project’s prediction model. This allows the team to estimate where outbreaks may occur. Kumar says their model now suggests that the virus can be detected up to four days before a clinical diagnosis of COVID-19. It also shows that the virus persists in wastewater up to five days after a positive diagnosis, he added.
 In addition, since the COVID-19 variants are now prompting more outbreaks, Solo-Gabriele says they are now also working with Mason to sequence and perform metagenomic analysis of some of the wastewater samples. This will allow them to figure out which COVID-19 variants are circulating on the University’s campuses.
In addition, since the COVID-19 variants are now prompting more outbreaks, Solo-Gabriele says they are now also working with Mason to sequence and perform metagenomic analysis of some of the wastewater samples. This will allow them to figure out which COVID-19 variants are circulating on the University’s campuses.
Streamlining the data
Meanwhile, co-investigator Stephan Schürer, a professor of molecular and cellular pharmacology at the Miller School, is also working with team member Dušica Vidović to streamline the massive influx of data coming from the sample collection process.
 Schürer and Chris Mader, director of applications and system development for the University’s Institute for Data Science and Computing, are using this information to create a dashboard that will provide information about potentially emerging COVID-19 hot spots to university leaders. Meanwhile, they are also sharing the information with a national database created by the NIH to compare results across all the U.S. institutions that are monitoring COVID-19 in wastewater.
Schürer and Chris Mader, director of applications and system development for the University’s Institute for Data Science and Computing, are using this information to create a dashboard that will provide information about potentially emerging COVID-19 hot spots to university leaders. Meanwhile, they are also sharing the information with a national database created by the NIH to compare results across all the U.S. institutions that are monitoring COVID-19 in wastewater.
“We are building the infrastructure so that all the data and results of the wastewater analysis will be processed, integrated, and made accessible through a dashboard,” Schürer says.
As the project has progressed, Solo-Gabriele says they are adding more data, like samples from a Miami-Dade County wastewater plant to correlate with local COVID-19 positivity data. This will help refine the computer model and broaden their understanding of local wastewater surveillance. It also allows them to scale up their research to see the amount of virus present in a sample of up to 800,000 people.
 The model could help researchers across the country move forward as another surge of COVID-19 happens or help them to monitor future viruses that can be shed through wastewater, according to Solo-Gabriele.
The model could help researchers across the country move forward as another surge of COVID-19 happens or help them to monitor future viruses that can be shed through wastewater, according to Solo-Gabriele.
“Especially in pandemic situations, we need to have real-time data collection, analysis, and prediction systems at our fingertips,” she says. “I wish we had this system at the beginning of the COVID-19 pandemic. But at least now we have it moving forward so that if the illnesses change, you can monitor that through wastewater.”
SOURCE: Story by Janette Tannen for Inventum, appearing in UM Miami Health News
FEATURED IMAGE: Walter Lamar, executive director of Facilities, Safety and Compliance for the Miller School of Medicine, sets up an autosampler device to collect wastewater outside Lakeside Village on the Coral Gables Campus.