University of Miami physicians and infectious disease experts are working together to sequence positive coronavirus tests to learn about the newest variant popping up across the globe.
As the world learns more about the omicron variant and its reach, researchers at the University of Miami are collecting available positive COVID-19 tests and sequencing them to determine whether the newest variant is present in South Florida.
So far, no omicron variant has been detected.
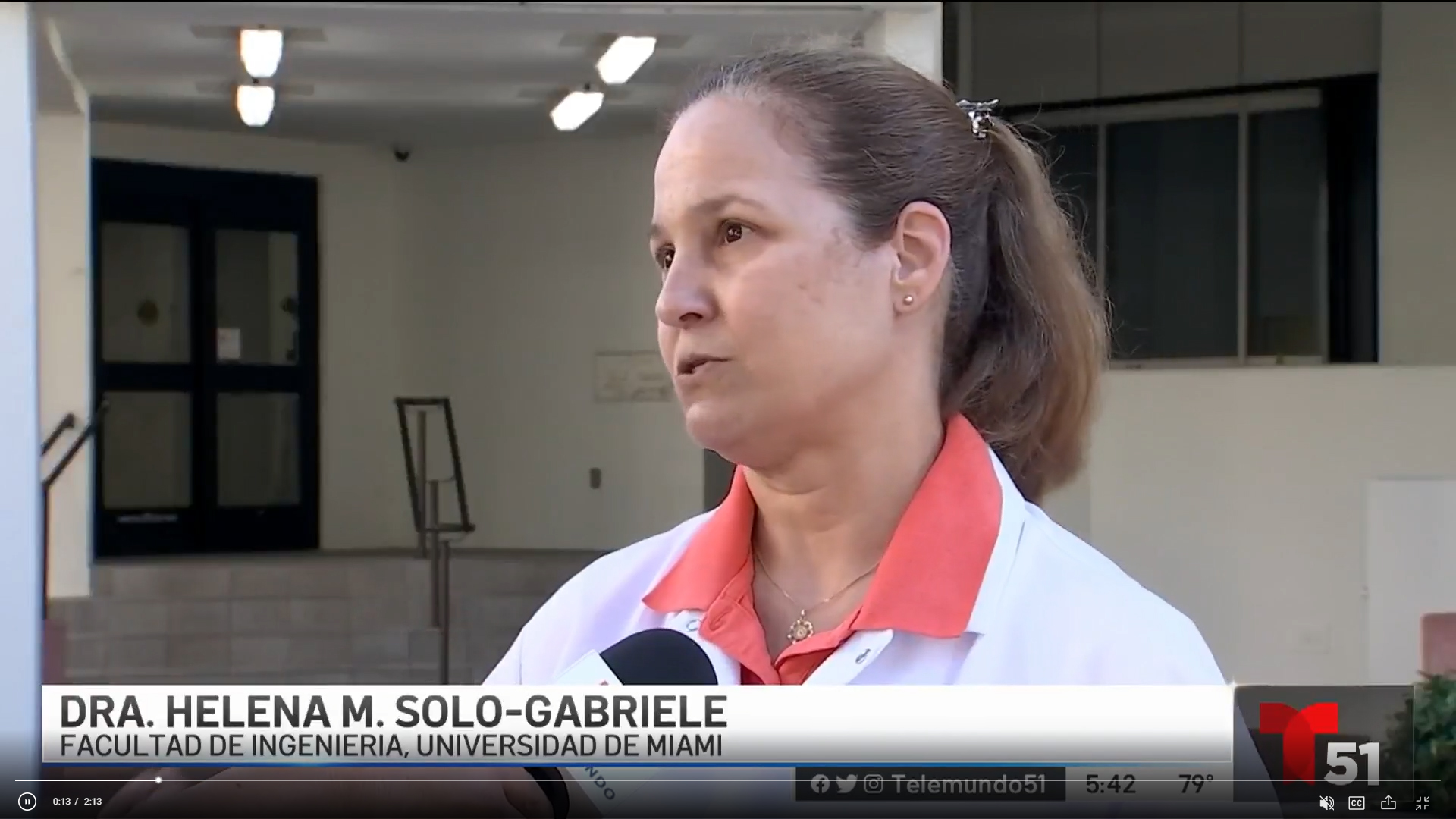
Dr. David Andrews, an associate professor in the Department of Pathology and Laboratory Medicine at the Miller School of Medicine, is leading the University’s variant tracking efforts.
On Nov. 26, his lab began taking COVID-19 positive samples from patients at UHealth Tower, Jackson Health System, and other locations and running them through an additional PCR test. This extra step helps reveal whether the sample has what is called a “spike gene target failure,” one distinguishing trait of the omicron variant.
The same test was also used to detect the alpha variant, first identified in the United Kingdom, so Andrews’ team is now well-versed in the technology. If a sample has this feature, it will be sent on for sequencing to determine whether it is in fact omicron.
“This is what most countries are doing to survey for omicron,” said Andrews, who also serves as vice chief of pathology for Jackson Health System.
Efforts to be expanded
His team will continue to process tests daily to learn whether the omicron variant is circulating in South Florida, and they hope to expand their efforts to include de-identified samples from local testing sites in the future.
“We expect to see omicron. And I hope to get an assortment of samples from across the county in the coming weeks, so that our lab can quickly find any early evidence of omicron, Andrews said.”
Identified by South African scientists near the end of November, the omicron variant is now present in more than 40 countries, including the United States where cases have been reported in at least 17 states so far. While new information emerges daily, scientists predict the variant likely arose in early November. Regardless, because of the more than 30 mutations on omicron’s spike protein—which is the vehicle for the novel coronavirus to enter human cells—its discovery prompted world leaders to quickly impose travel restrictions to help contain the spread.
A few of the University’s infectious disease experts explained some of the unique qualities of the omicron variant that may shed light on why many scientists and national leaders are so concerned.
Professor Mario Stevenson is a virologist in the Miller School’s Division of Infectious Diseases and directs the Institute of AIDS and Emerging Infectious Diseases. He cautioned that there is still much to learn about omicron and that most of the news right now is anecdotal.
“The next weeks and months will tell us where it came from, how it spreads, the symptoms, the breakthrough levels—if there are any—and all of that information will help us get a clearer picture of what we are dealing with,” he said.

Mutations cause concern
Still, Andrews, Stevenson, and his colleague, Dr. Dushyantha Jayaweera, a professor of medicine in the Division of Infectious Diseases, said there are a few mutations of the omicron variant that are of concern.
To understand the impact of a new variant, one needs to think about how viruses work, Stevenson explained. Viruses cannot exist on their own, so they depend on our body’s cell machinery to thrive. In the case of the novel coronavirus, the virus enters a human’s lung or nasal cells when its spike protein attaches or binds to an ACE 2 receptor found in human cells. This exchange opens the door for the virus to enter our bodies and spread by replicating itself.
Vaccines provide an extra hurdle for the virus because they stimulate the body to produce antibodies that can block the spike protein from entering human cells, Stevenson pointed out. Also, if for some reason the antibodies fail, vaccines also help build T-cells in the body’s immune system. These T-cells recognize infected cells and then attack and kill them, he added.
Yet when the COVID-19 vaccines were created, scientists used the genetic makeup of the spike protein found in the original novel coronavirus from Wuhan, China. And each time there are mutations to the spike protein—like those found on omicron—the virus strays farther from the version that the vaccine was created to thwart.
“It’s like there’s a few more holes in the Swiss cheese that the vaccine may not be able to close,” Andrews said. “The vaccine will probably still protect us; it may just be less effective.”
Clues about omicron

While they wait for more scientific data to be shared globally about omicron, Stevenson said he and other molecular biologists are watching how the new variant is spreading through the population. This could reveal how dangerous it is—or isn’t, he noted.
In a place like South Africa, where just 36 percent of the population is vaccinated against COVID-19, it is easy for a virus like omicron to spread, Stevenson said. But how omicron behaves in a place where there are high rates of vaccination and high levels of the delta variant, like in South Florida, may be a different story. According to Andrews, the last few sequencing runs demonstrated that nearly all UHealth and Jackson Health System patients with COVID-19 had the delta variant.
“If there are high rates of vaccination and the delta variant in a region, and omicron starts spreading quickly through the population, that would be a cause for concern, because that may signal that omicron will outcompete the delta variant . . . and the mutations it has are the sorts of mutations that would allow it to do that,” Stevenson said.
Silver Linings
So, how can we prevent omicron from fueling yet another COVID-19 surge? Andrews, Jayaweera, and Stevenson all agree: vaccines and boosters.
“Vaccination is the key to getting out of this mess and it’s important that we vaccinate the rest of the world, too,” Jayaweera said. “Because if we think we can get away with only vaccinating our population in the U.S., it’s a fool’s paradise.”